A 45 year old with shortness of breath, cough
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and prognosis
A 45 year old male, labourer by occupation, came to the OPD with
Chief complaint-
- Shortness of breath since 3 days
- Cough since 30 days
- Generalised body swelling since 20 days
- Whitish urine since 15 days
History of presenting illness-
- Patient was apparently asymptomatic 30 days back, then developed cough which was insidious in onset, gradually progressive and was associated with sputum which is whitish, foul smelling, and scanty in quantity
-There was generalised swelling till knees since 5 months
- there was history of shortness of breath on walking a short distance (100 meters) since 2 months
Past history-
- history of DM-2 since 10 years
- history of HTN
- not a known case of thyroid, asthma, epilepsy, CAD, TB
Treatment history-
- Inj. Human Actrapid Insulin
- Tab Nicardia
Personal history-
- Appetite - normal
- Diet - mixed
- Bowel and bladder movements - Normal
No known allergies
No known addictions
Family history :
Not significant
GENERAL PHYSICAL EXAMINATION:
Patient is conscious, coherent and cooperative, oriented well to space and time.
Well nourished and well built.
Pallor - not seen
Icterus - not seen
Cyanosis - not seen
Clubbing - not seen
Lymphadenopathy - not seen
Pedal edema - putting type, seen upto level of the knees
VITALS :
Temperature - Afebrile
Pulse rate - 80 bpm
B.P - 120/80 mm of Hg
Respiratory rate - 18 cpm
SpO2 - 98% at room temperature
Systemic Examination:
1) CVS :
S1, S2 heard;
apex beat heard
no thrills or murmurs heard
2) Respiratory System:Dyspnoea - No
Wheeze - No
Position of trachea - central
Respiratory sounds - Vestibular
No abnormal sounds detected
On inspection ‐
Chest is bilaterally symmetrical
Expansion of chest: Equal on both sides
Position of trachea: Central
No visible scars, sinuses, pulsations
On palpation :
Expansion of chest was equal on both sides.
Position of trachea: Central
Tactile Vocal Fremitus: resonant note was felt.
On percussion: all lung areas were resonant
On auscultation :
Bilateral air entry was present, normal vesicular breath sounds were heard.
Vocal resonance: resonant in all areas
3) Per Abdomen -
Scaphoid abdomen, no tenderness, no palpable mass and free hernial orifices seen.
No free fluid in the abdomen , no bruits
Liver and spleen not palpable
Normal bowel sounds heard
4) CNS - All higher mental functions are intact
Motor System examination
Tone
Upper limb
-Hypertonia in both right and left lower limb (3/5)
Power
-Upper limbs - in right and left grade 3
-Lower limbs - in right and left grade 2
Reflexes
-Biceps - Normal in both right and left
Triceps - Normal in both right and left
Supinator - Normal in both right and left
Knee jerk reflex - Not elicited
Ankle jerk reflex - Not elicited
Plantor reflex - Not elicited
CEREBELLAR SIGNS :
Finger nose test -abnormal
Heel knee test -abnormal
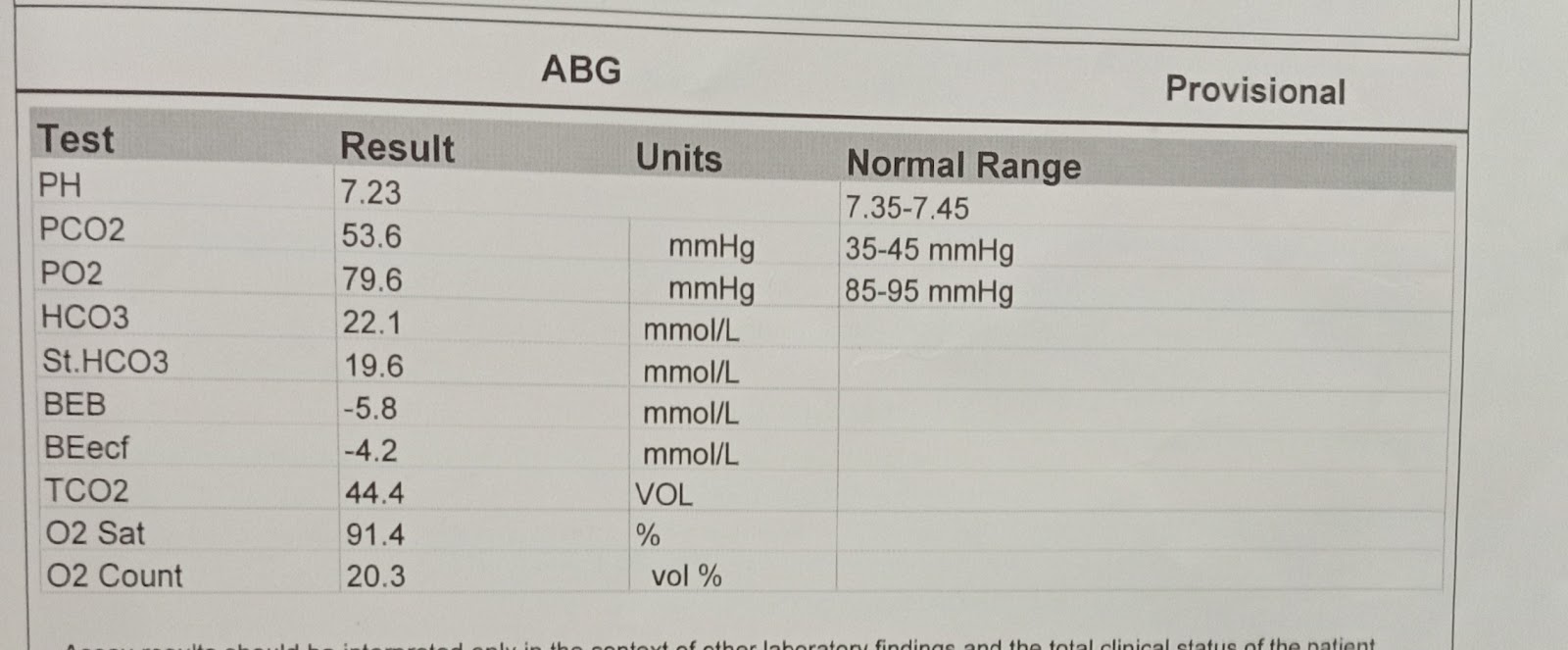
Provisional Diagnosis:
Chronic Kidney Disease on Maintenance haemodialysis.
Paraparesis
Investigations :
ECG
Treatment :
Maintenance haemodialysis.
Salt restriction < 2 grams per day
Fluid restriction < 1.5 liters per day
Tab. DROFER
Inj. HAI sc TID
Tab. Nicardia 20 mg
Inj. EPO 4000 IU sc. 2 x weekly
Inj. Iron sucrose in 100 ml NS